Copyright 2024
Medical Security Card Company, LLC
All Rights Reserved
WellRx will never sell your personal information. Period. By signing up I agree to WellRx's terms of use and privacy policy.
By Jillian Foglesong Stabile, MD
August 31, 2023
Insomnia is a serious medical condition. Up to one-third of patients who go to see their primary care physician may experience intermittent troubles with sleep, and up to 10 percent may have persistent trouble sleeping. Insomnia can involve difficulty falling asleep, difficulty staying asleep, early awakening, or non-refreshing sleep. Daytime consequences of insomnia include fatigue, decreased energy, difficulty concentrating, irritability, lost work productivity, and sometimes accidents.
Insomnia carries a significant economic burden. The direct and indirect costs of insomnia are conservatively estimated at over $92 billion annually. These costs are related to medical care, accidents, hospitalizations, absenteeism, decreased productivity, increased morbidity and mortality, increased depression, and increased substance abuse. With costs this high, it’s important to know how to identify and treat this complex medical problem. Many patients who suffer from sleep problems don’t bring it up to their healthcare provider. The first step in evaluating and discussing this serious medical condition is to talk with your healthcare provider.
Insomnia can be defined by the length of time the symptoms have been present.
Acute insomnia is usually caused by some significant emotional or physical stressor. It can last anywhere from 1 night to about 4 weeks before it is considered chronic. Acute insomnia can be caused by disruption of your normal biological rhythm, such as with jet lag, or by illness or significant life stressors. Environmental factors such as noise, light, and temperature can also play a role.
Chronic insomnia is defined as insomnia that occurs 3 or more times a week for at least a month. This type of insomnia can be caused by one or more factors acting alone or in combination. It is also associated with other medical problems.
Less than half of cases of chronic insomnia are caused by psychiatric, medical, or neurological disorders. Anxiety and depression are associated with insomnia as well as schizophrenia. Heart and lung problems, chronic pain, reflux, urinary problems, and immobility can cause sleep disruptions. Other medical conditions such as pregnancy, perimenopause, and menopause can also cause difficulty with sleep. Patients who have dementia can also have significant disruption to their sleep cycles.
There are many prescription medications and other substances that can affect sleep quality and sleep cycles. Drugs of abuse such as heroin, cocaine, and stimulants can disrupt sleep cycles. Prescription drugs such as antidepressants, steroids, decongestants, beta blockers, caffeine, alcohol, and nicotine can affect sleep as well. They affect patients differently, so not everyone will have the same responses to these medications. Over-the-counter medications such as allergy medications can disrupt the sleep cycles.
While insomnia is itself a sleep disorder, other specific sleep disorders can contribute to insomnia:
Primary insomnia is insomnia that is not associated with any of the other causes of insomnia. This can be associated with poor sleep habits, chronic stress, or hyperarousal.
Insomnia is generally a clinical diagnosis, which means that there are no specific tests or imaging studies for it. Certain tests can be used for some of the other conditions associated with insomnia such as sleep apnea. The diagnosis of insomnia is made primarily based on history: medical and psychological as well as sleep history. If you are going to be talking with your doctor about possible insomnia, keeping a diary of your sleep and your symptoms can help facilitate this conversation.
Because insomnia is a complex, multifactorial problem, it often requires a multifactorial approach to treatment. If there is an underlying condition such as sleep apnea, this can sometimes be treated without medication. Sleep apnea specifically can be treated with continuous positive airway pressure (CPAP). For insomnia that doesn’t have an easily treated underlying medical cause, there may be other non-pharmacological options for treatment.
Behavioral interventions are effective and recommended as the initial line of treatment for insomnia. There are several approaches to behavioral interventions.
Sleep hygiene is a common initial intervention and doesn’t necessarily require supervision by your healthcare provider. Sleep hygiene involves removing and adjusting the personal habits and environmental factors that affect sleep. This includes limiting alcohol, caffeine, and nicotine for at least four to six hours before bedtime. Use the bedroom only for sleep and sex, maintain a regular sleep-wake cycle, and avoid daytime napping. You should also avoid loud noises, bright lights, and extreme temperature variations at bedtime. Studies have shown that this therapy is superior to placebo, but the exact effectiveness is not clear.
This type of therapy is designed to establish regular sleep-wake cycles and to associate the bedroom with sleep. The recommendations for this type of therapy include things like lying down to sleep only when feeling sleepy. Use the bedroom for sleep and sex. Avoid television in bed. Leave the bed if you can’t fall asleep within 20 minutes and come back when sleepy. Avoid daytime naps. Set the alarm for the same time every morning regardless of how much sleep occurs. All of these techniques are designed to establish a regular sleep cycle and trigger your brain to recognize the cues for sleep.
This is best for patients who spend a lot of time in bed trying to fall asleep. The patient should limit the time in bed to the number of hours they actually spend sleeping. This should start with no less than 5 hours and then gradually be increased as sleep efficiency improves.
CBT-I is best for older adults and patients who chronically take hypnotic medications. Studies have shown it to be significantly better than some medications for the treatment of chronic insomnia. CBT-I is a combination of sleep restriction therapy and stimulus control therapy. It may also include relaxation therapy as well as writing down daily thoughts and working to change misconceptions, beliefs, and attitudes that can affect sleep.
Paradoxical intention is a method in which the patient is taught to confront their fear of staying awake by intentionally staying awake and accepting the state of quiet wakefulness until they can fall asleep.
Several over-the-counter treatments for insomnia are available that people try from time to time. About a quarter of people with insomnia take over-the-counter sleep aids.
Antihistamines are usually marketed for allergies but may also be marketed for insomnia. Diphenhydramine and doxylamine are two commonly advertised medications for sleep. Studies have shown that these medications are only minimally effective, can reduce sleep quality, and can cause residual sleepiness on awakening.
Many herbs and dietary supplements are marketed for sleep. Of the many options, only melatonin and valerian root have been shown to help. Melatonin is a naturally occurring hormone produced in the brain. It is involved in sleep regulation and helps with changes in circadian changes. It is also approved for the treatment of circadian rhythm disorders in blind children and adults. There isn’t much information about the long-term safety of this herbal treatment. Valerian root affects a neurotransmitter called GABA. There isn’t a lot of information about insomnia, but it does cause sedative effects in the brain.
Alcohol certainly causes sedation but is not recommended for insomnia. It can cause problems with certain aspects of the sleep cycle. It has a high potential for abuse, so it is not recommended.
Many medications can be prescribed for insomnia. Your healthcare provider can guide you as you work together to decide what medication is best for you, but we’ll do a brief overview of the classes of medication available.
Barbiturates are medications that affect the GABA receptor in the brain. They are not recommended for chronic insomnia use because they negatively affect aspects of the sleep cycle. They are sometimes used in the short term (2 weeks or less). Opiates are not recommended for sleep due to their abuse potential and their effects on the sleep cycle. However, they may treat specific painful conditions that may be interfering with sleep. Some antidepressants are used for sleep. They can decrease the length of time you get to sleep and increase wakefulness after sleep onset. They are best used in patients who have depression in addition to their insomnia.
These medications have long been used to treat sleep. They can increase sleep time and improve sleep quality, but they also can cause some of the same issues as alcohol because they interact with the same receptors in the brain. They also have the potential for addiction and abuse. Withdrawal from these medications can cause anxiety, depression, nausea, rebound insomnia, intense dreams and nightmares, and memory problems.
These medications are newer and affect the same receptors as benzodiazepine. They have fewer effects on the sleep stages, so they have benefits. They can still cause problems with memory and slow responses. Some of these medications can cause increased problems with things like sleepwalking and sleep eating.
There are a couple of other medications in newer classes, such as ramelteon and suvorexant. These medications affect different parts of the brain. They have a lower likelihood of physical dependence, but are newer, so may be more expensive.
Insomnia, like any chronic condition, can affect multiple parts of your life. The long-term effects can be health and life-threatening. Addressing insomnia and its comorbid conditions can be life-changing for patients. Before starting any prescription or nonprescription treatment for your insomnia, you should talk to your healthcare provider about treatment options and possible underlying conditions that affect your sleep cycles.
Dr. Foglesong Stabile is a board-certified Family Physician who enjoys full scope Family Medicine including obstetrics, women’s health, and endoscopy, as well as caring for children and adults of all ages. She also teaches the family medicine clerkship for Pacific Northwest University of Health Sciences.
References:
https://www.aafp.org/pubs/afp/issues/1999/0601/p3029.html
https://pubmed.ncbi.nlm.nih.gov/7859246/
https://www.nhsinform.scot/illnesses-and-conditions/mental-health/insomnia
https://www.aafp.org/pubs/afp/issues/2015/1215/p1058.html
https://www.aafp.org/pubs/afp/issues/2007/0815/p517.html
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4400203/pdf/nihms-635936.pdf

For your convenience, use the ScriptSave® WellRx mobile app. Now savings are well in hand, right at the pharmacy counter. Save on your family's prescription medicines.
Learn More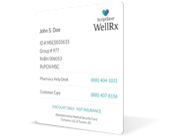
Your choice. Get a ScriptSave WellRx Savings Card. Or Download the free mobile app from the App Store or Google Play Store
Get A Card
ScriptSave WellRx Grocery Guidance leverages leading-edge nutritional data science to help you know which food products on your grocery store shelf are truly good for YOU.
Healthy Foods For YouTags:

November 07, 2024

October 23, 2024

May 07, 2024
You need to log into the site to use this feature
This feature requires registration. Sign up or log in to your free WellRx account to gain access to this and other tools to help make managing your medications and wellness easier.
Benefits Include:
 Store & manage your medication list
Store & manage your medication list
 Medication pricing updates
Medication pricing updates
 Medication information
Medication information
 Pill & refill reminders
Pill & refill reminders
 Medication journal & mood log
Medication journal & mood log
This feature requires registration. Sign up or log in to your free WellRx account to gain access to this and other tools to help make managing your medications and wellness easier.
Benefits Include:
 Store & manage your medication list
Store & manage your medication list
 Medication pricing updates
Medication pricing updates
 Medication information
Medication information
 Pill & refill reminders
Pill & refill reminders
 Medication journal & mood log
Medication journal & mood log
You will be redirected to your program in 5 seconds.
Our Terms and Conditions and Privacy Policy have recently been updated.
By declining you will be logged out of your account